According to a United Nations report, soon there will be more 60-year-olds than 15-year-olds in our society.
It’s the result of fewer births and lengthening life span. The U.S. Census shows more and more people are living to age 100: the centenarian population has increased 65.8 percent in the past three decades (1980–2010). America has more than 55,000 centenarians; close to 6,000 live in California. Yet with this extended longevity comes a series of questions on how people living more years can have quality of life. With old age comes uncertainty. As evolved humans, we don’t just want to live longer, we want to age well.
If you’ve been tuning in to the topic of optimal aging, you might be wondering: how do we protect our cells’ proteins from mutating, folding inside out and creating sticky toxic plaque? How do we keep the microbiome in our digestive tract in balance? How do we prevent our immune system from running amok and declaring unnecessary battle on our body? How do we ensure that we can remember our grandchildren’s names when we are 90?
When it comes to chronic illness (like cardiovascular disease, cancer and Alzheimer’s), age itself is one of the most powerful causative factors. Thankfully, doctors, scientists, researchers and great minds around Marin County and throughout the world are studying the mechanisms underlying aging and developing potential ways to reverse the processes that lead to chronic disease.
“The work being done at the Buck Institute for Research on Aging increases the possibility of intervening in the aging process,” says Brian Kennedy, Ph.D., president and CEO of the institute. “Aging is the biggest risk factor for many diseases; therefore, success in slowing aging will likely make people healthier later in their life span.” Here are some of the compelling findings on cognitive ability, gut health and immunity, telomere lengthening, cellular homeostasis and longevity — all processes that, if optimized, can result in graceful aging.
The Brain and Aging
One of the troubling by-products of growing old is dementia — an estimated 44 million around the world now suffer from it. Some estimates say 160 million people worldwide could be afflicted by 2050, with more than 7.7 million new cases reported globally each year (that’s about one new case every four seconds). The numbers are daunting, as is the image of Julianne Moore in the movie Still Alice. Billions have been spent on research and clinical trials, but many unanswered questions remain. One thing we know for sure: aging causes dementia and cognitive decline. And Alzheimer’s is on the rise; 5.3 million Americans now have the disease.
“The reality is that 15 percent of us in America will get Alzheimer’s,” says Dr. Dale Bredesen, an internationally recognized expert in neurodegenerative diseases and founding CEO of the Buck Institute. So of the 300 million living in the U.S., 45 million will develop Alzheimer’s disease (AD) — it’s just that most people are simply too young to know it yet, Bredesen says.
So what do we know about this progressive brain disorder that slowly destroys memory and thinking skills and has historically been irreversible?
Scientists are discovering that age-related changes in the brain such as atrophy, synapse loss and free radicals may contribute to AD, as does genetics. Apolipoprotein E (ApoE), a cholesterol-carrying protein that transfers fat, is also involved in AD. It’s encoded by the gene of the same name. “This gene has several forms but it’s ApoE4 that’s troublesome,” says Bredesen’s colleague Ram Rao, a Ph.D. and associate research professor at the Buck.
Apparently, about two-thirds of people with AD carry ApoE4, and women who carry the gene are more likely to get AD than men are. The gene is also linked to formation of the amyloid-beta peptide associated with sticky plaque, one of the supposed hallmarks of the disease, but how ApoE4 actually brings or heightens risk for the disease is unclear.
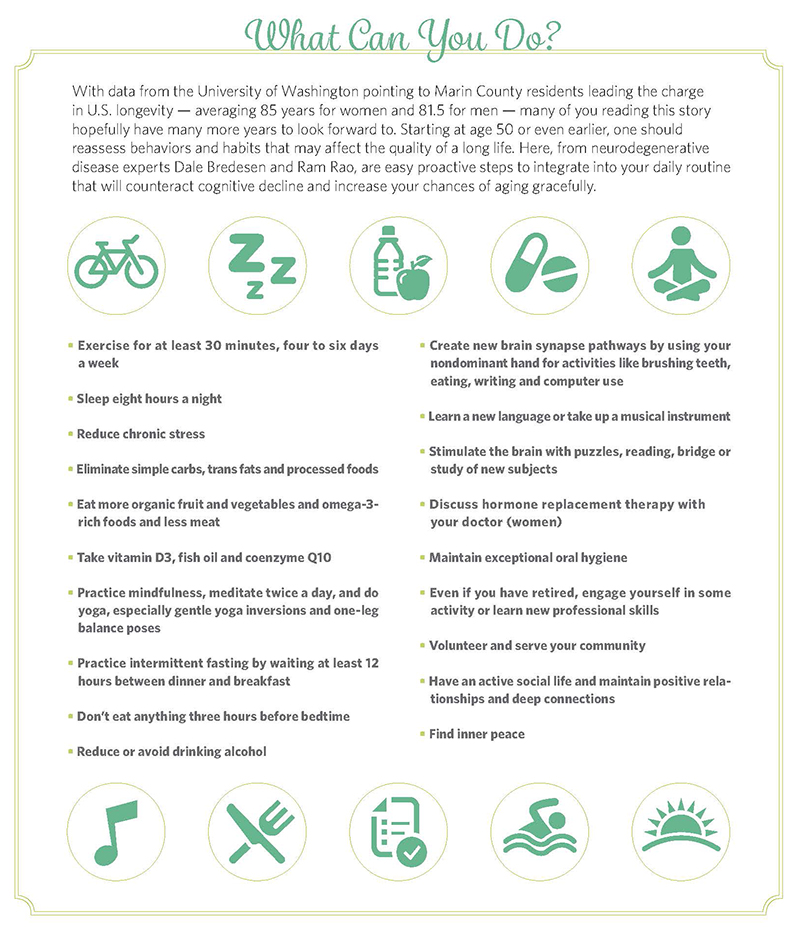
Even though ApoE4 is considered a major genetic risk factor for AD, Rao doesn’t recommend rushing out to get tested for it: “Having one or two copies of the ApoE4 gene does not mean that an individual will develop Alzheimer’s disease. Similarly, not having the ApoE4 gene does not guarantee that the individual will not have the disease.” That’s the case even with a family history of Alzheimer’s disease, he says. “Furthermore, testing for this gene would be more problematic,” he adds. “It could cause unwarranted fear, worry and anxiety about getting the disease. Genetic tests are of value only in a research setting. Instead, I would advocate for anyone above 50 to do all the (recommended) lifestyle
interventions irrespective of their ApoE4 status” — everyday regimen changes that can help prevent cognitive decline (see sidebar).
What’s more, says Bredesen, studies he’s involved in through the UCLA Mary S. Easton Center for Alzheimer’s Disease Research and the Buck Institute suggest cognitive decline can be reversed. That will take a broader-based treatment rather than searching for a single drug with a single target, the research suggests. Tackling or preventing cognitive decline requires changes in factors like diet, exercise, stress exposure, sleep, brain stimulation and vitamin intake. AD sufferers commonly have insulin resistance, vitamin D abnormalities, inflammation issues, and hormonal imbalance, Bredesen says. “I tell people, ‘Now that you are having problems with your memory, we are going to treat you like a competitive athlete.’ We want people to be optimal, not just normal.”
One of the first recommendations for patients with cognitive decline is exercise, which can slow the progression, alleviate depression, improve quality of life and even help prevent AD itself. Diet also plays a big role. In fact, Bredesen says, the fastest track to Alzheimer’s would be eating a ton of sugar to spike your insulin; gobbling up trans fats, simple carbs, processed foods and beef with hormones; and avoiding vegetables and fruits — and to drive the nail in the coffin, be sure to drive everywhere and get no exercise. Other risk factors include poor hygiene, high stress and lack of sleep.
“There’s also a window of 10 years from first symptoms until we can no longer reverse it,” he adds. If AD is detected early on, there’s still time to counteract detrimental effects. But most people arrive at a clinic with symptoms when they’re beyond that 10-year window.
Meanwhile, researchers at the Queensland Brain Institute have shown that noninvasive ultrasound can restore memory in mice with AD, by breaking apart the neurotoxic beta-amyloid plaques in the brain they think cause cognitive decline. Sound waves opened the mice’s blood-brain barrier and stimulated microglial (waste-removal) cells to eradicate the beta-amyloid clumps. Memory function was fully restored in 75 percent of the mice without damaging brain tissue. The study’s co-author, Professor Jürgen Götz, believes this method could “revolutionize Alzheimer’s treatment.” The Australian team hopes to scale the treatment to higher animal models such as sheep and then conduct human clinical trials.
But Rao questions whether such technology can be replicated in more complex animals or people. “Until now, nearly all of the rodent findings could not successfully be translated in humans,” he notes. “When it comes to exposing the human brain to ultrasound waves (even at low intensity), there are safety concerns. There is always a danger of triggering a massive immune reaction or causing brain hemorrhage. Besides, AD researchers are still unsure whether eliminating beta-amyloid deposits (by any type of intervention) is the key to treating or stopping Alzheimer’s.”
Another study co-authored by Bredesen and Rao at the Buck Institute has revealed a correlation between ApoE4 and SirT1, an “antiaging protein.” ApoE4 causes a dramatic reduction in SirT1, as seen in both neuron cells and in brain samples from people with AD. “Through identifying drug candidates that increase SirT1, abnormalities such as creation of phosphotau and amyloid-beta associated with ApoE4 and AD could potentially be prevented,” says Rao. “This research offers a new type of screen for Alzheimer’s prevention and treatment.” The same study also revealed that resveratrol, the antioxidant in red wine, can increase SirT1 levels — another affirmative vote for that evening glass of cab, in moderation of course.
While strides are clearly being made, larger trials are needed to support the findings in Bredesen’s research and to determine whether Alzheimer’s treatments that seem to succeed with mice can help people.
Telomeres and Longevity
Turns out sometimes bigger is better — at least with telomeres, the protective microscopic shields at the end of our chromosomes that preserve our genetic information. With each cell division (most cells can replicate 50 times), the DNA is copied and the telomeres shorten. If telomeres get too short, the cell can no longer divide and becomes inactive or dies. Healthy people have long telomeres; unusually short telomeres can be predictors for disease, even death. And while most would assume the telomeres of all older people are short, the length of telomeres can actually fluctuate in individuals.
Dr. Elizabeth Blackburn received the Nobel Prize in medicine in 2009 for discovering how chromosomes are protected by telomeres and the enzyme telomerase, which repairs and rebuilds them. At Yale she studied a one-celled organism, tetrahymena, and deciphered the structure of telomeres, which she likens to the caps on the tips of shoelaces that keep them from fraying over time. She found the enzyme while working with a grad student on her team at UC Berkeley in 1984.
Now a professor of biology and physiology at UC San Francisco, Blackburn has continued her research, linking shortened telomeres to diseases like cancer, diabetes and heart disease. For the past 13 years her work with Elissa Epel, a UCSF psychologist, has studied connections between telomeres and stress. They found shorter telomeres and decreased telomerase in spouses who were caring for mates with dementia and in mothers of children with chronic diseases.
So how do we lengthen our telomeres and build telomerase? Studies have shown that people following a Mediterranean diet tend to have the healthiest telomeres, because of the diet’s oxidative and anti-inflammatory effects. Exercise is a great stress buster. And studies by Blackburn and others show that by counteracting stress and promoting well-being, meditation and mindfulness block the shortening of telomeres. At the Shamatha Project, a three-month intensive meditation retreat, Blackburn and UC Davis researchers found telomerase activity in participants’ white blood cells was one-third higher than in a control group’s.
Meditation may also cause positive changes in the brain itself: in a Harvard-affiliated study in 2011, MRI scans of participants in a mindfulness meditation program showed greater gray-matter density in the hippocampus, a brain area associated with stress, empathy, memory and sense of self. A 2015 UCLA study suggests meditation might help preserve gray matter as well. Such structural changes confirm the brain’s plasticity (ability to change as a result of behavior or other external factors), though further research is needed.
That meditation lowers stress symptoms is clear: it can slow heart rate, lower blood pressure and fortify the immune system. For people who find it hard to sit still, Rao suggests simply quieting the mind for two minutes and easing into longer sessions from there. Thirty minutes twice a day is optimal, according to the Chopra Center in Carlsbad, California. While that may sound tricky to fit into a daily schedule, “if you say you don’t have time for meditation, then you are definitely the type of person who needs it most,” Deepak Chopra points out.
The bottom line: exercise, meditation and yoga may boost telomerase and lengthen telomeres, potentially resulting in a longer life.
The Gut
Our digestive system literally has a mind of its own. It’s controlled by the enteric nervous system, which Columbia University neurogastroenterology expert Michael D. Gershon calls “the second brain.” This complex system (about nine meters long from entry to exit) has 500 million neurons — more than the spinal cord. It sends and receives impulses, communicates with other body systems, responds to emotions and has 30 major neurotransmitters, including serotonin and dopamine, that influence wellness and mood. Ninety-five percent of the body’s serotonin can be found in the bowels.
Much of our immune system (70 percent) and its response are regulated by the gut, or belly brain. Trillions of microorganisms live in our gut, mouth, skin and body, collectively comprising our human microbiome. They digest food, synthesize nutrients and vitamins, and stop disease-causing bacteria from invading the body. Microbiome research is recognized as one of the most important emerging fields in biomedical research. The health of one’s microbiome may play a significant role in overall health, affecting conditions such as autoimmune disorders and obesity.
In patients with diseases like irritable bowel syndrome and Crohn’s, gut microbiome is often less diverse, altered by our low-plant-fiber Western diet and antibiotics. Scientists are excited by recent success with fecal microbiota transplants (FMT), transfer of healthy fecal matter into ailing patients, notably those with clostridium difficile (C. diff), a bacterial infection acquired after antibiotics, often in hospitals, that kills more than 15,000 people a year. In a trial published in The New England Journal of Medicine, 94 percent of C. diff patients who received FMT recovered. “It’s the closest thing to a miracle I’ve seen in medicine,” said gastroenterologist Zain Kassam, interviewed in a New Yorker piece called “The Excrement Experiment” last December.
Can managing gut health and one’s microbiome prevent disease and lengthen life? Research has connected changes in gut bacteria with cancer, diabetes, inflammatory bowel and age-related disease. In a study headed by Heinrich Jasper, professor and chief science officer at the Buck, scientists altered the gut bacteria of fruit flies, which significantly increased their life span. The bacterial load in fly intestines had increased dramatically with age, causing an inflammatory condition and production of free radicals that can lead to a precancerous state. “Our study explores age-related changes in the gut that include increased oxidative stress, inflammation, impaired efficiency of the immune response, and the overproliferation of stem cells,” he says. Increasing the expression of PGRP-SC, the molecules that regulate the immune response to bacteria in the intestinal epithelium (a response that can be mimicked by drugs), restored microbial balance and halted overproiferation of stem cells, increasing life span. The study supports the idea that the right microbiome balance is vital to wellness and longevity.
It’s not yet known whether diet can significantly strengthen the microbiome, Jasper adds. But probioticrich foods like kefir, yogurt, kimchi, kombucha and miso may help keep the gut in balance.
Cell-Signaling Pathways
The immunosuppressant drug Rapamycin also shows promise as a longevity-extending agent. The Buck’s Kennedy is conducting research on cell-signaling pathways, in particular the mTOR pathway, which senses cellular nutrients, oxygen and energy levels and tells cells whether to grow, divide or stop. When cells are constantly active, he explains, they can spew toxic free radicals. Kennedy hopes to determine whether pathways like mTOR can be regulated to prevent or treat aging-related disease. Studies of mice show Rapamycin has a “robust” effect on life span, extending it by 30 percent even in rodents of advanced age.
Rapamycin is already in use for human organ transplant patients, but it has considerable side effects, and Kennedy emphasizes no one is talking about prescribing it for longevity just yet. But the implications for aging humans are intriguing. In one groundbreaking study, a group of healthy people 65 and older took a derivative of Rapamycin for six weeks, followed by flu vaccine two weeks after stopping the drug. “Rapamycin was tolerated by healthy older people and it improved their reaction to the influenza vaccine,” Kennedy says. But it can also “suppress the immune system and effect insulin resistance,” he adds. “We need a new derivative of this drug.” Still, the study “certainly sets the stage for future clinical trials of drugs that show promise to (one day) improve the health of older adults.”
Protein Homeostasis
The importance of protein homeostasis — an organism’s ability to maintain the proper structure and balance of its proteins — is another hopeful area of research. In a Buck Institute study, Gordon Lithgow, Ph.D., found that Thioflavin T (aka ThT or Basic Yellow 1), a dye used in labs to detect damaged proteins in Alzheimer’s, extended life span in healthy nematode worms by more than 50 percent and slowed Alzheimer’s in worms bred to mimic aspects of the disease.
“A protein is a long molecule that has to take a certain shape to function,” Lithgow says. “Most proteins take the right shape and do their jobs. But as we age, a lot of proteins take a different shape — they don’t fold correctly or they unfold and do damage. They can also stick to each other, becoming insoluble,” one of the hallmarks of Parkinson’s disease.
Since many degenerative diseases are linked to breakdown in protein homeostasis, it’s encouraging that ThT supports homeostasis instead — especially given that genetic studies show it contributes greatly to longevity in complex animals. “We have been looking for compounds that slow aging for more than 10 years, and ThT is the best we have seen so far,” Lithgow says. It also “slows the clumping of toxic protein fragments,” which may explain another way it can extend life span.
Other research is highlighting the life-extending powers of lithium, a drug normally prescribed for bipolar disorder. “We stumbled across it when working with worms,” Lithgow says. While lithium is toxic in high concentrations, there’s a “sweet spot” where it’s beneficial. Buck Institute scientist Julie Andersen, Ph.D., an expert in Parkinson’s, has also observed positive effects of low-dosage lithium in older mice having a Parkinson’s mutation, suggesting more research is warranted to see if it can help humans with the disease.
“I think aging research is at a tipping point,” Lithgow says. “In the labs we are seeing unbelievable changes in organisms — age-related diseases are disappearing, life spans are extending, and we are starting to understand the mechanisms (of aging), so there’s lots of promising stuff. Translating this to humans is a whole different story and takes years. But we should be excited about it as a society.”

Ann Wycoff is a travel and lifestyle writer whose work has appeared in San Diego Magazine, Coastal Living, Modern Luxury, and many more. She lives in Encinitas, CA with her husband and daughter, and believes in traveling with a purpose.