Our world has changed radically in the past six weeks. Suddenly, seeing your doctor quickly switched from an in-person event to a matter of logging into your computer. Telemedicine is now a main source of health care.
Telehealth had originally been intended as a way of reaching rural communities with a shortage of doctors. As a result of the COVID-19 pandemic, in the past month, video visits with healthcare providers have become common practice in all kinds of communities around the country. At Ann & Robert H. Lurie Children’s Hospital of Chicago, the number of telemedicine visits has increased 500% since the onset of the national health emergency.
We talked with healthcare providers about the changes, their benefits and how to make the most of the telehealth appointments you and your family may have.
What Changed to Allow Telemedicine To Take Off Suddenly
As the number of COVID-19 cases skyrocketed, the risks of visiting a doctor in person and the importance of staying home also escalated dramatically. For telemedicine to happen on a large scale, both the federal and state governments had to take action. They did so, and quickly.
At the federal level, the government relaxed the Health Insurance Portability and Accountability Act (HIPAA) privacy rules, which were designed to protect patients’ medical records and other health information. The Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS) said that health care providers could expand their services despite the fact that doing so may not fully comply with the rules and it would not impose penalties for noncompliance.
“We are empowering medical providers to serve patients wherever they are during this national public health emergency,” states Roger Severino, OCR Director, on the HHS website. The CDC also recommended use of telehealth options to reduce the volume of people seeking care outside their homes.
The extent to which telehealth visits were permitted and reimbursed by insurance varied by state, too. As the virus spread, many governors took action to make telemedicine widely available. In an executive order on March 19, Illinois Governor J.B. Pritzker required insurers to cover the costs of telehealth services, including health care and mental health services provided by video technology and by telephone, the same way they would in-person visits. Governor Gavin Newsom of California signed a similar executive order that facilitated the expansion of telemedicine on April 3.
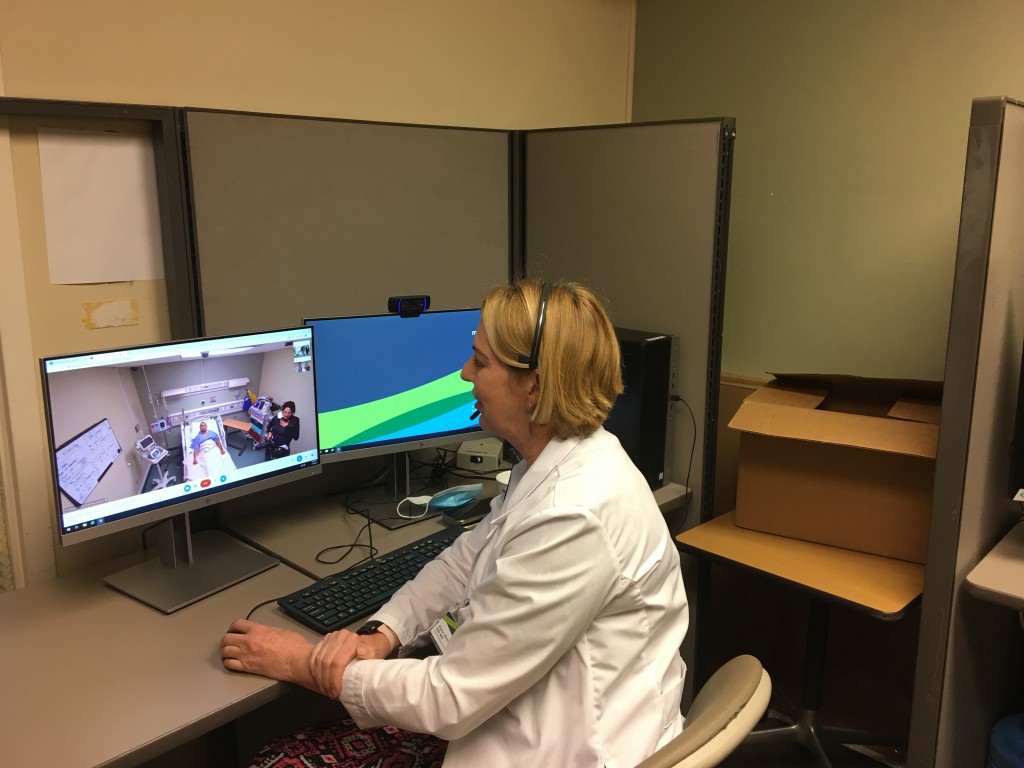
While those changes happened very quickly, many health care systems have been working for years to implement telemedicine. “This is a big shift in medicine,” says Karin Reese, Chief Nursing Officer at MarinHealth in Marin County, California. She has been working on implementing telehealth for five years. “This crisis has shown that we can quickly adapt and make those changes, and some of the people who may have been initially resistant to this change are now big adopters,” she says. “It’s been a tremendous paradigm shift.”
Benefits of Telemedicine
Both providers and patients have jumped into this new realm and are seeing a myriad of benefits. Telemedicine has taken off because it can help reduce the spread of the COVID-19 virus. It allows clinicians to see their patients without the risk of contagion, which protects health care workers, office staff and other patients by limiting their interaction and chances of exposure to the virus.
Logging in does not require suiting up, and therefore telemedicine minimizes the need for personal protective equipment (PPE). That is particularly true in hospitals that are using telemedicine. Reese explains that individuals like pharmacists and rehabilitation therapists who need to interact with the patient but not necessarily in person can do so via a video feed that shows the caregiver’s face on the television in their room. That eliminates the need for any PPE for them. It also makes it possible for nurses to check in with the patient to see what their needs may be prior to entering the room so they can have every item they need, rather than having to go in and out of the room several times, each time requiring additional PPE.
Connecting through telemedicine at home also has big benefits during the pandemic. It “enables us to offer continuity of care for patients, but it also keeps them from accessing care from through other channels — like emergency departments and urgent cares — reducing the stress on the healthcare system during this difficult time,” explains Joan Berta, Director of Physicians Practice at Shirley Ryan AbilityLab in Chicago.
For patients connecting with doctors at home, the convenience factor of telemedicine is a tremendous benefit. Kimberly Brennan, PT, Administrative Director, Outpatient Therapy and Specialized Services at the Shirley Ryan AbilityLab, thinks that convenience “could help lead to better compliance with physician and therapy visits, and positive outcomes as a result.”
Brennan notes that another benefit is that by seeing patients in their homes, their physical therapists and other clinicians “have been able to create exercise plans and recommend equipment to help patients navigate in specific environments. This access has been especially valuable within our pediatric population, as kids’ behaviors and motivating factors are often different in their home environments than in traditional physician and therapy sessions.”
Peace of mind is another benefit, with several health care providers mentioning that the ability to counsel patients has been a big part of their practice the past few weeks. Patients have been grateful to connect safely with a trusted professional.
Things to Consider
While there are clear benefits to this new approach to care, “not everything will fit in the realm of telemedicine,” Dr. Gregory Wallman, D.O., internist at NorthShore University HealthSystem, cautions, noting that there are some conditions that require a physical exam.
Dr. Dana Schinasi, MD, Medical Director of Telehealth Programs at Ann & Robert H. Lurie Children’s Hospital of Chicago, agrees. “Telemedicine has its place, but it is to augment care and not intended to replace in-person care. It is not always right for every patient or every condition,” she says.
Although the HIPAA regulations are relaxed, privacy is still a consideration when it comes to telehealth. Clark said that he does not have concerns when interacting via phone and that it is important to make sure “only an accepted, compliant platform is utilized” for video visits. All providers said their platforms are secure and that information is encrypted. They noted that while there is a live stream of video, nothing is recorded.
Wallman says that he balances privacy concerns with the patient’s health. “Making sure they get the medical care they need is what is most important,” he says.
The ability to use that technology is also necessary for video visits from home, though providers report that patients are much more comfortable after connecting with family, friends and colleagues using video technology such as Zoom, Skype and FaceTime. Those interactions have also alleviated some worry about being on camera that some patients have had, though Schinasi notes that it was not an issue for kids, who often love being on camera.
If technology use or access is a problem, telehealth visits can also happen via the phone. Wallman says some patients who struggle with technology are using the phone instead.
Richard Clark, MD, FAAFP, family medicine at Northwestern Medicine Grayslake Outpatient Center, says most of his recent visits have been conducted by telephone. “Although I miss the opportunity to see people in person, and fully recognize that these visits do not include thorough physical exams, I have been heartened by the ability to maintain contact with and help my patients during this very challenging time,” he says.
Tips for Making the Most of a Telehealth Visit
The physicians we spoke with offered some suggestions for making your telemedicine appointment as effective as possible.
- Be aware that you may be contacted prior to the visit. Some practices email information in advance. Clark’s staff contacts patients by phone prior to their appointment to obtain information such as updates to medications and vital signs.
- Familiarize yourself with the platform your provider is using. Some doctors use Skype, others use a videoconferencing option available through a patient portal such as MyChart. Allow time to familiarize yourself with the platform before your visit.
- Don’t feel like you need to clean up. Don’t worry, no one is judging your housekeeping skills. Natasha Burgert, pediatrician in Overland Park, Kansas, assures parents of her little patients that sweatpants are completely fine.
- Let there be light. Providers are not looking closely at your home, but they do want a good look at you. Burgert suggests sitting near a window for natural light, or in a bathroom with bright lighting. Have a flashlight nearby. It can be helpful for looking in throats and illuminating skin issues.
- Be as respectful and observe boundaries just as you would at an office visit. Schinasi notes that you wouldn’t record or take photos of a doctor conducting an exam during an office visit, so don’t do so during a video visit.
- Take advantage of other ways to stay well and stay at home. Burgert notes that many patients are reaching out to her to determine the difference between seasonal allergies and viral infections, such as a cold or the COVID-19 virus. She notes that when it is allergies, she recommends “over-the-counter treatments, including long-acting non-drowsy antihistamines. Often, these types of medications are available for delivery, so you don’t need to risk an unnecessary trip to the pharmacy.” Do as much as you can from home and limit the number of trips out.
What the Future of Telemedicine Looks Like
When life returns to normal, it’s unclear what will happen to the rules currently enabling telemedicine, which are good only for during this public health emergency. The physicians we spoke with all emphatically said that they hope and expect telemedicine can continue when the crisis is over. “When we come out of this, telemedicine will become a major player in primary care,” Wallman predicts.
“We’ve shown that we are capable of providing care via telemedicine, and now that patients have experienced it, we believe there will be a demand,” says Schinasi, who notes that there will still be medically fragile patients who will benefit from being able to see their doctor without traveling and exposure to other illnesses.
Reese anticipates that we will look at telemedicine “in a whole new light in nine months.” She adds, “My hope for the future is that we have gained early adopters who will keep an open mind and start to look at how we can be more efficient and how we can provide excellent patient care in an environment that’s only getting more difficult.”
More from Marin:
- Quarantined With COVID-19: Marin County’s Public Health Officer Shares His Experience
- Surfing During COVID-19: How to Be a Responsible and Eco-Friendly Surfer
- Our Elderly and COVID-19: What to Know, What to Do and How to Help At-Risk Seniors During the Coronavirus Outbreak
 Shannan Younger is a writer living in the western suburbs of Chicago with her husband and teen daughter. Originally from Ohio, she received her undergraduate and law degrees from the University of Notre Dame. Her essays have been published in several anthologies and her work has been featured on a wide range of websites, from the Erma Bombeck Humor Writers Workshop to the BBC. She also blogs about parenting at Between Us Parents.
Shannan Younger is a writer living in the western suburbs of Chicago with her husband and teen daughter. Originally from Ohio, she received her undergraduate and law degrees from the University of Notre Dame. Her essays have been published in several anthologies and her work has been featured on a wide range of websites, from the Erma Bombeck Humor Writers Workshop to the BBC. She also blogs about parenting at Between Us Parents.